Perhaps you have heard of ‘leaky gut’ syndrome. More and more people suffer from digestive problems, skin irritations, food intolerances or chronic fatigue without knowing that it all starts in the gut. Your gut is not only responsible for digestion, but also acts as a protective shield. When this barrier becomes permeable, substances that do not belong there enter the bloodstream – and your immune system reacts. In this article, you will learn exactly what leaky gut syndrome is, what causes it and what you can do to strengthen your intestinal wall again.
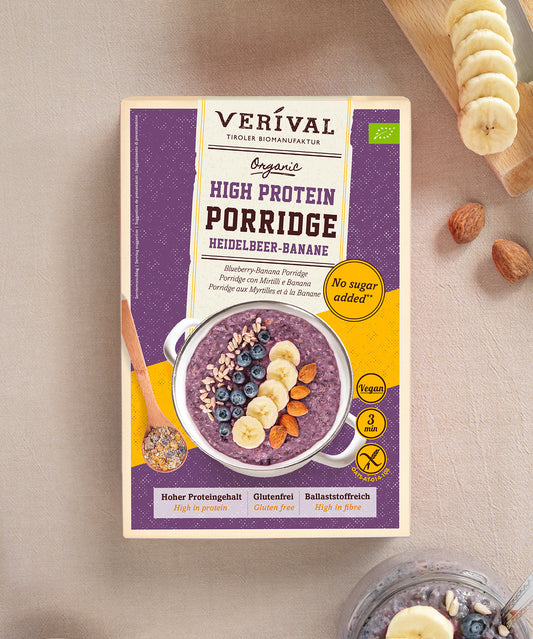
Discover and celebrate the entire Verival breakfast range here!
What does ‘leaky gut’ actually mean?
The term leaky gut refers to a disorder of the intestinal mucosa in which the natural protective barrier between the inside of the intestine and the rest of the body is weakened. This barrier consists of a single layer of cells – known as enterocytes – and is normally tightly sealed by tiny connections called tight junctions. These ensure that only nutrients and water can pass through, while harmful substances, bacteria and toxins remain outside.
How the barrier works – and why it is so important
When healthy, your gut regulates very precisely what passes through the mucous membrane into the bloodstream. This function is vital, as enormous amounts of food particles, microorganisms and chemical substances flow through your digestive tract every day. Your gut constantly decides what your body is allowed to absorb – and what is recognised as potentially dangerous and must be rejected.
With leaky gut, this finely tuned system becomes unbalanced. The tight junctions become permeable, allowing undigested food residues, bacterial components and toxins to enter the bloodstream. Your immune system recognises them as foreign substances and reacts with inflammation.
What happens in the body when the intestine ‘leaks’
This process often goes unnoticed for a long time, but can cause numerous complaints: flatulence, bloating, food intolerances, skin problems or constant exhaustion. The development of autoimmune diseases is also associated with leaky gut, because the permanent activation of the immune system overwhelms the body.
A permeable intestine is therefore not an isolated problem – it affects the entire system. The first step towards healing is to understand the causes. Because only when you know what is weakening your intestine can you take targeted action to counteract it.
What are the most common causes of leaky gut?
The gut does not simply become ‘leaky’ because it suddenly loses its function. It is a gradual process caused by many small stresses – and that is precisely where the problem lies. The causes are varied, but they can usually be traced back to a few main factors: diet, stress, medication and environmental pollution.
The interplay of many small triggers
Often it is not one cause, but a combination. A diet high in sugar with heavily processed foods, regular alcohol consumption and too little fibre disrupts the microbiome – i.e. the balance of your gut bacteria. This imbalance weakens the mucous membrane and opens the ‘gates’ in the intestinal wall.
Stress is another factor. If you are under constant pressure, your body produces more cortisol, which reduces blood flow to the intestinal mucosa and slows down its regeneration. Lack of sleep, lack of exercise and certain medications – such as painkillers, antibiotics or proton pump inhibitors – also attack the intestinal barrier.
Why modern lifestyles put strain on the gut
Our everyday lives are demanding, and this is directly reflected in our guts. Eating quickly, not getting enough rest, ready-made products, soft drinks, alcohol and environmental toxins such as pesticides or heavy metals upset the delicate protective layer. Even seemingly harmless things such as excessive coffee consumption or constant dieting can have the same effect in the long term.
To protect your gut, you need to make several changes: adjust your diet, reduce stress, get enough sleep and be mindful of your medication. This is the only way for the intestinal barrier to recover.
Unhealthy diet & sugar traps
Diet is one of the biggest factors influencing the development of leaky gut. Your gut is sensitive to what you eat every day. An unbalanced diet with too much sugar, white flour, processed fats and artificial additives weakens the intestinal barrier in the long term. It alters the microbiome, irritates the mucous membrane and promotes silent inflammation – often without you noticing it immediately.
Sugar – the invisible enemy of your gut health
Sugar is hidden in countless foods: in sauces, muesli, spreads and even in supposedly ‘healthy’ yoghurts. If you regularly consume too much of it, you are not only feeding your energy needs, but also unfavourable gut bacteria. These multiply rapidly and displace the protective species that would normally strengthen your intestinal wall. This leads to dysbiosis – an imbalance in the microbiome – and it is precisely this dysbiosis that is one of the main triggers of leaky gut.
Sugar also causes blood sugar fluctuations, which increase inflammatory processes in the body. If your insulin levels are constantly fluctuating, mucosal regeneration also suffers. Your gut loses its ability to repair itself after stress.
Processed foods and additives – stress for the intestinal mucosa
Many ready-made products contain not only sugar, but also emulsifiers, preservatives, flavour enhancers and colourings. These additives can attack the mucous layer that protects the inner wall of your intestine and make it more permeable. Emulsifiers found in low-fat products or baked goods are particularly problematic – they disrupt the structure of the tight junctions, i.e. the cell connections that seal your gut.
Low-quality fats also play a role. Trans fats, such as those found in fried foods or industrially produced snacks, promote inflammation and put additional strain on your digestion and intestinal health. Over time, tiny micro-injuries develop in the mucous membrane – small tears through which unwanted substances can enter your bloodstream.
How you can protect your gut with nutrition
The good news is that you can reverse these processes. A fibre-rich diet with plenty of fresh vegetables, healthy fats (e.g. from linseed oil, avocado or nuts) and fermented foods such as sauerkraut or kefir strengthens your microbiome. Consistently reduce your sugar intake and focus on natural, unprocessed foods. This gives your intestinal wall the chance to regenerate and become resilient again.
Medications & their effects on the intestinal wall
Medications can save lives, there's no question about that. But many of them also attack the sensitive structure of your intestinal mucosa – especially if you take them over a long period of time. Your gut is very sensitive to chemical substances, and certain medicines can weaken the barrier, promote inflammation or upset the balance of your microbiome.
Antibiotics – both a blessing and a burden
Antibiotics are one of the biggest disruptive factors for your gut flora. They destroy not only harmful bacteria, but also the beneficial ones that protect your mucous membrane and aid digestion. Even a single course of antibiotics can throw your microbiome out of balance for weeks or even months. During this time, you lack protective intestinal bacteria, and pathogens or yeasts can multiply more easily. This weakens the mucous membrane and opens the door to leaky gut syndrome.
If you have to take antibiotics, you can support your gut by consuming probiotic foods or specific supplements at the same time – but always consult your doctor first.
Painkillers, acid blockers & co – underestimated triggers
Frequently used medications such as ibuprofen, aspirin or diclofenac can also irritate the intestinal mucosa. They inhibit certain enzymes that are actually responsible for mucus production, and it is precisely this mucus that protects your intestinal wall from stomach acid and digestive enzymes. If this protective layer becomes thinner, the mucous membrane can literally ‘fray’.
Another problem: proton pump inhibitors (PPIs), which are often used to treat heartburn. They reduce stomach acid – which sounds pleasant at first – but it is precisely this acid that is necessary to kill pathogens and break down proteins properly. Without it, microorganisms can enter the intestine more easily, which increases the risk of dysbiosis and leaky gut in the long term.
If you take medication regularly, it is worth protecting your gut in a targeted manner – through a high-fibre diet, sufficient fluids, mild herbal teas and conscious breaks between treatments.
Chronic stress & excess cortisol
Stress is almost an everyday occurrence these days. Appointments, obligations, constant availability – all of this challenges your nervous system every day. Your body responds by releasing stress hormones such as cortisol and adrenaline. In the short term, this is not a problem, as this reaction is designed to keep you performing at your best. But when stress becomes chronic, your hormone balance changes – and this has a direct effect on your gut.
How stress weakens your gut
Your gut is in close contact with your brain. The two communicate constantly via the so-called gut-brain axis. When you are stressed, your body releases cortisol – and this hormone ensures that energy in the form of glucose is made available to enable a ‘fight or flight’ response. At the same time, however, digestive processes are slowed down.
This means that blood flow to your intestinal mucosa decreases, nutrients are absorbed less efficiently, and the regeneration of mucosal cells slows down. Over time, this makes the barrier thinner and more susceptible to irritants, germs or inflammation.
In addition, chronic stress changes the composition of your microbiome. Studies show that under chronic stress, protective bacteria decrease while pro-inflammatory species increase. This creates an imbalance that promotes what is known as ‘leaky gut’.
Excess cortisol – the silent saboteur
If your body releases too much cortisol over weeks or months, the entire system becomes unbalanced. Cortisol has an anti-inflammatory effect – but only in the short term. In the long term, permanently elevated cortisol levels weaken your immune system and disrupt the repair mechanisms of the intestinal mucosa.
The tight junctions, i.e. the tiny protein connections between the intestinal cells, become unstable. This allows toxins, undigested food components or bacterial residues to enter the bloodstream. The body reacts to this with inflammation, fatigue, skin problems or even mood swings – all typical symptoms of leaky gut.
What you can do to combat stress in the gut
Your gut needs rest periods, just like you do. Try to incorporate regular short breaks into your daily routine – conscious breathing, going for a walk or short meditation sessions can help to calm the nervous system. Sleep also plays a crucial role, as both the microbiome and the intestinal mucosa regenerate at night.
In addition, foods rich in magnesium (e.g. oats, pumpkin seeds, spinach) and B vitamins help to reduce stress. And: listen to your body. If you notice that you are constantly under pressure or tension, it may be a good idea to seek professional help – your gut will thank you for it too.
Alcohol & environmental toxins as a burden
Many people underestimate how much alcohol and environmental toxins can stress the gut. They have a subtle but profound effect. Your gut is in daily contact with everything you eat, drink and breathe – and this is exactly where the problem begins. While a healthy intestinal mucosa normally reliably wards off harmful substances, constant contact with alcohol or toxins weakens its structure. The result: The protective barrier becomes permeable, inflammation spreads, and the risk of leaky gut increases significantly.
How alcohol attacks the intestinal wall
Alcohol has several negative effects on your digestive tract. Even in small amounts, it can reduce mucus production, which normally protects the intestinal wall from acids and bacteria. This makes the mucous membrane more sensitive and susceptible to micro-injuries.
At the same time, alcohol promotes the formation of so-called reactive oxygen compounds (free radicals), which cause oxidative damage to your intestinal cells. This becomes particularly critical with regular or excessive consumption – then even the tight junctions, i.e. the cell connections that stabilise the intestinal barrier, change.
What's more, alcohol alters your microbiome. Studies show that the proportion of protective bacteria such as Lactobacillus and Bifidobacterium decreases, while pro-inflammatory species increase. This leads to chronic irritation of the mucous membrane – and that is the ideal breeding ground for leaky gut.
Environmental toxins – the invisible attackers
It's not just alcohol; environmental toxins also have a massive impact on your gut. Pesticides, heavy metals, microplastics and plasticisers enter your body via food, air and packaging. They can trigger inflammatory reactions, alter the microbiome and hinder the regeneration of the mucous membrane.
Certain chemicals from plastics, such as BPA (bisphenol A), are particularly problematic. This substance has a hormone-like effect and can directly weaken the intestinal barrier. Pesticide residues from conventional agriculture are also considered stress factors because they inhibit beneficial intestinal bacteria and at the same time hinder the liver's detoxification performance.
How you can protect yourself
Environmental toxins cannot be completely avoided – but you can significantly reduce your exposure to them. Choose unprocessed, organic foods wherever possible, drink plenty of water (preferably filtered) and avoid plastic packaging whenever you can. Bitter substances – such as those found in dandelions, artichokes and chicory – also support the liver in detoxification and thus indirectly relieve your intestines.
If you drink alcohol, do so consciously and in moderation. Your gut needs time to regenerate – and it can only do so if you give it breaks. Every alcohol-free day is a step towards a stronger intestinal barrier and better health.
Fibre-rich Verival breakfast – discover it here!
Imbalance in the microbiome (dysbiosis)
Your gut is its own little ecosystem. Billions of microorganisms live here – bacteria, fungi and even viruses – and together they form your microbiome. This system is finely tuned: good and potentially harmful bacteria keep each other in balance so that your digestive system functions smoothly. When this balance is disrupted, dysbiosis occurs – and this is precisely one of the main triggers of leaky gut syndrome.
How dysbiosis develops
Dysbiosis rarely develops overnight. It is caused by many small factors that add up: too much sugar, industrially processed foods, medication, alcohol or constant stress. Lack of sleep and lack of exercise also play a role. These influences change the living conditions in the gut – and thus also the composition of the bacterial community.
Protective strains such as Lactobacillus or Bifidobacterium, which normally strengthen your intestinal mucosa, are displaced. Instead, pro-inflammatory bacteria multiply. These produce metabolic products that irritate the mucosa, alter the pH value and promote small areas of inflammation. Over time, this weakens the tight junctions – the microscopic connections that seal your intestinal wall.
The result: the mucous membrane loses its stability. Foreign substances, bacterial fragments or undigested food components can enter the bloodstream and trigger immune reactions there. Many people feel the consequences in the form of flatulence, diarrhoea, skin blemishes, fatigue or food intolerances – without knowing that the real problem lies in the microbiome.
Why the microbiome is so important for your immune system
Around 70 per cent of your immune cells are located in the gut. This is where it is decided whether a substance is classified as harmless or a threat. A healthy microbiome ensures that your immune system reacts in a balanced way – not too sluggishly, but also not overactively.
But when the balance is disturbed, your body loses this control. It overreacts – for example, with chronic inflammation or autoimmune reactions. At the same time, it finds it more difficult to effectively ward off pathogens. This explains why many people with dysbiosis are more susceptible to infections or feel constantly exhausted.
How you can strengthen your microbiome again
The good news is that your microbiome is flexible. With the right diet and lifestyle, you can restore the balance. Fibre from vegetables, oats, flaxseed or psyllium husks is like ‘food’ for the good bacteria. Fermented foods – sauerkraut, kimchi, kefir or kombucha – also provide living microorganisms that promote the diversity of your intestinal flora.
Also make sure you get enough rest, regular exercise and sufficient sleep. Your microbiome loves rhythm – too much chaos in your everyday life is also reflected in your gut. And above all: give your body time. A stable gut flora does not develop overnight, but through consistent, conscious decisions in everyday life.
Infections & chronic inflammation
Not only diet and stress, but also infections and persistent inflammation can severely weaken the intestinal barrier. Your digestive system is in constant contact with billions of microorganisms – many of them beneficial, some potentially dangerous. If this interaction becomes unbalanced, your immune system reacts – and if this reaction becomes too strong or too frequent, the intestinal wall suffers.
How infections attack the mucous membrane
Acute infections – caused by viruses, bacteria or parasites, for example – temporarily throw your digestive system out of balance. You may remember times when you were sensitive to certain foods for weeks after suffering from gastroenteritis or food poisoning. This is because infections can damage the mucous membrane.
Any inflammation in the intestine causes the tight junctions – the tiny cell connections that seal the intestine – to open up. This happens so that immune cells and antibodies can intervene more quickly. Normally, these connections close again once the infection has subsided. However, if new stimuli are added, such as stress, sugar or medication, the mucous membrane remains permanently weakened – and this is precisely the beginning of leaky gut.
Sometimes, chronic low-grade inflammation triggered by recurring infections, an imbalance in the microbiome or irritants in the diet is enough. These silent inflammations often go unnoticed, but have a long-term destructive effect on the intestinal mucosa.
Chronic inflammation – the breeding ground for leaky gut
Chronic inflammation occurs when your immune system remains permanently on alert. Instead of calming down after an infection, it continues to produce pro-inflammatory messenger substances such as cytokines. These attack the mucosa, alter the composition of bacteria and make the intestinal wall even more permeable.
A classic example is irritable bowel syndrome or inflammatory bowel diseases such as Crohn's disease or ulcerative colitis – these involve inflammatory processes that can cause lasting changes to the intestinal structure. But even people without a clear diagnosis can suffer from such silent inflammation.
The result: the body reacts more sensitively to certain foods, digestion becomes unsettled and symptoms such as flatulence, bloating, skin problems or exhaustion occur.
What you can do about infections and inflammation
To protect the gut, it is important to support the immune system without overburdening it. An anti-inflammatory diet rich in antioxidants (e.g. from berries, green leafy vegetables, turmeric and ginger) helps to stimulate the healing process. Omega-3 fatty acids from flaxseed, chia seeds or fish also have a soothing effect on the mucous membrane.
Rest, sufficient sleep and conscious relaxation are also crucial – they reduce stress hormones and promote regeneration. And if you suffer from frequent infections or intestinal problems, it is worth having your microbiome professionally analysed to find out which types of bacteria are out of balance.
Lack of sleep & lifestyle factors
A healthy gut needs more than just a good diet. It also needs rest, exercise and regular periods of relaxation. But this is often neglected in modern everyday life. Too little sleep, irregular meals, sitting for too long and constant stress from deadlines throw your body out of sync – and this has a direct impact on your gut health.
Why sleep is so important for your gut
While you sleep, your body works at full speed. It repairs cells, reduces inflammation and strengthens the immune system. The regeneration of your intestinal mucosa also mainly takes place at night. So if you regularly sleep too little or restlessly, you miss out on these important renewal phases.
Studies show that even a few nights of poor sleep can alter the composition of the microbiome. Protective bacteria decrease, while those that promote inflammation increase. In addition, cortisol levels rise, which, as you already know, weakens the tight junctions and makes the intestinal barrier more permeable.
Lack of sleep often goes hand in hand with cravings for sugar and fatty snacks, which further exacerbates the situation. Your body is looking for quick energy, but it is precisely these foods that promote inflammation in the gut.
Lifestyle factors that upset the balance of the gut
It's not just sleep; your daily behaviour also has a direct impact on gut health. Lack of exercise is one of the biggest risk factors for digestive problems. Regular exercise — even moderate walking — stimulates bowel activity, improves blood flow to the mucous membrane and strengthens bacterial diversity in the gut.
Another point: irregular meals. If you constantly snack between meals or eat carelessly, your digestive system doesn't get any breaks. But these breaks are important so that the gut can cleanse and regenerate itself.
Smoking, excessive caffeine consumption and constant screen work also have a negative effect. They promote oxidative stress, strain the liver and disrupt hormonal regulation – a vicious circle that weakens the gut in the long term.
How you can make your everyday life more gut-friendly
It's not about living perfectly, but more consciously. Plan regular sleep times, treat yourself to exercise in the fresh air and take time to eat. Switch off screens at least an hour before bedtime, drink enough water and try to structure your day with little islands of calm – five minutes of breathing exercises, a cup of herbal tea or simply a few deep breaths outdoors can already help.
When you slow down your daily routine, your gut benefits too. It reacts sensitively to your stress levels, your diet and your rhythms. Balance is the key word here – and it starts with conscious self-care.
Discover our healthy Verival snacks here!
Conclusion: Recognising the causes – first steps towards a healthy gut
Leaky gut does not develop overnight. It is the result of many small stresses that accumulate over weeks, months or even years – unhealthy diet, stress, lack of sleep, medication, alcohol, environmental toxins or infections. Each of these factors contributes to your intestinal barrier losing its stability. But the good news is: you can strengthen it again.
The first step is awareness. Once you recognise the triggers in your life, you can take targeted countermeasures. An gut-friendly diet with fresh, natural foods, sufficient fibre and fermented products supports the regeneration of your mucous membrane. Regular sleep, exercise and stress-reducing routines are just as important – your gut needs relaxation as much as it needs nutrients.
Even small changes make a difference: less sugar, less alcohol, and more mindfulness when eating and in everyday life. Your gut responds to every signal you give it. When you start nurturing it instead of stressing it, you will quickly notice how not only your digestion but your overall well-being improves.